Core Clerkship
Mission Statement:
To provide a Surgical Curriculum that applies consistently to all clerkship sites in order to include comparable educational experiences and equivalent methods of assessment across all instructional sites and to support a learning environment that fosters professional competence within a culture that prepares students for international medical practice.
To emphasize, review and integrate the student’s knowledge of basic scientific information with clinical material to result in favorable educational outcomes in the acquisition of knowledge regarding the etiology, pathophysiology, diagnosis, treatment, and prevention of surgical diseases.
To emphasize to the students the integration of the basic sciences in the development of current clinical knowledge in conjunction with ongoing changes in surgical treatment and technology.
To provide students with the tools for life-long adult learning of surgical diseases for their ongoing professional development.
COURSE GOALS and OBJECTIVES
1. MEDICAL KNOWLEDGE
- Discuss the presentation and treatment of diseases that are commonly addressed within the field of surgery.
- Identify how and when evidence-based information and other aspects of practice-based learning and improvement affect the care of the surgical patient and the alternatives in management.
- Discuss cost to benefit ratio, the role of payment and financing in the healthcare system, the role of multi-disciplinary care including ancillary services such as home-care and rehabilitation and other aspects of systems-based practice in the implementation of the available technologies used in surgical treatment.
- Demonstrate understanding of the Core Topics (modules listed below) and its application to associated surgical knowledge in clinical analysis and problem solving.
- Utilize distributive learning through the use of on-line resources for surgical learning and problem-solving.
2. CLINICAL SKILLS
- Apply the principles of surgical practice, including operative and non-operative management to common conditions.
- Apply the tools of clinical problem solving for surgical conditions including the process of data collection (history, physical examination and laboratory and imaging studies) in establishing a list of differential diagnoses and a primary working diagnosis for treatment and further investigation.
- Identify the importance of and approach to informed consent for surgical operations and procedures, with emphasis on the risks, benefits, and alternatives.
- Demonstrate application of interpersonal and communication skills in the multidisciplinary care of the surgical patient in an environment of mutual respect.
- Demonstrate the ability to conduct proper sterile preparation and technique.
3. PROFESSIONAL BEHAVIOR
- Function as a part of the surgical care team in the inpatient and outpatient setting.
- Demonstrate proper behavior in the procedural setting, including the operating room, at all times.
- Recognize the limits of one’s position within the surgical care team in order to appropriately engage each patient, their friends and associates and their family.
- Appropriately seek supervision as provided through the hierarchical structure of the surgical care team.
- Identify and respond sensitively to cultural issues that affect surgical decision-making and treatment
- Develop an understanding of and approach to the principles of professionalism as they apply to surgery through the observation of the role-modeling provided by the surgical faculty.
- Demonstrate responsibility and compliance by fulfilling rotation expectations and participating in all required learning activities.
1. Length: 12 weeks.
- General Surgery, for up to 8 weeks students will be incorporated into a surgical team for a broad clinical experience. Students on surgery will also have dedicated education time. During these weeks student on-call experience is recommended. The specific on-call model will be at the discretion of the Clerkship Director, recognizing the balance between valuable clinical learning opportunities and students’ need for independent study time.
- The sub-specialty experience should be for 1 to 2 weeks for each component and may include Anesthesiology, Bariatric Surgery, Cardiothoracic Surgery, Emergency Medicine, Neurosurgery, Ophthalmology, Oral and Maxillofacial Surgery, Orthopedic Surgery, Otolaryngology, Pediatric Surgery, Plastic Surgery, Podiatry, Surgical Critical Care, Transplant Surgery, Trauma Surgery, Urology and Wound Care as well as other procedure oriented sub-specialties. The selection and time distribution of the associated sub-specialty experience will be at the discretion of the Clerkship Director.
2. A specific formal orientation session, at the start of the clerkship must be provided.
The orientation must include the behavioral expectations for each student, including a discussion of professional behavior and interpersonal and communication skills as well as an overview of the departmental organization and the facilities of the site.
Student schedules must be provided as well as assignments to residency teams and preceptors. The Clinical Training Manual must be provided as a reference within the orientation process indicating the location on the SGUSOM website. A review of the Goals and Objectives, Clerkship Guidelines and evaluation process should be conducted.
3. Inpatient, outpatient and acute care experience should be provided.
4. Attending rounds for house staff and students should be conducted at least three times a week.
5. The clerkship must include a schedule of teaching conferences, both in conjunction with and in parallel to the educational opportunities of the residents/registrars, including grand rounds, subspecialty conferences and didactic sessions that address the Core topics of the Clinical Training Manual. Students should be encouraged to study at least 3 hours every evening and at least 8 hours on weekend days off.
Protected Study Time
- There should be direct preceptor supervision of the students at least three hours per week with case presentations by the students and bedside rounds, including physical examination and interactive sessions. The Standard Departmental Examination format and cases that are distributed at each clinical meeting may be used for teaching as well as for formative and summative feedback, particularly in the assessment of clinical reasoning, problem solving and communications skills.
- A sufficient number of comprehensive write-ups are required over the course of the clerkship to ensure student competency in documentation of a comprehensive history and physical exam. The “Patient Encounter Template” that is distributed at each faculty meeting is based on the USMLE Step 2 CS examination and is recommended. The exercise should be structured to address the development of Clinical Skills through a defined problem solving approach with data gathering based on: 1) clinical history, 2) physical examination and 3) laboratory, imaging and other ancillary studies in order to develop: 4) a rank-order differential diagnosis list and concluding with 5) a primary working diagnosis to discuss with the patient and will direct treatment, prognosis and/or further investigation. Formative feedback on the exercise must be part of the process. Oral presentations are also required and student competency in their ability to present pertinent findings during rounds and preceptor sessions is assessed.
- Electronic patient encounter logs are to be maintained and up to date at all times. (Instructions regarding the log are found in Section One of the Clinical Training Manual)
- Electronic patient logs should be periodically inspected by the Clerkship Director and at mid-rotation in order to monitor the types of patients or clinical conditions that students encounter and modify them as necessary to ensure that the objectives of the education program are met. The patient logs may also be used by the Dean and the Chair of Surgery in order to monitor the types of patients or clinical conditions that students encounter in order to determine if the objectives of the medical education program are being met.
- Students will be responsible for the review of basic anatomy, pathology and physiology of all surgical problems encountered.
- Department of Surgery is responsible to teach and assess competency in starting an intra-venous line and venipuncture.
Evaluations:
In addition to formative feedback given within the daily progress of the 12-week rotation, a defined formative feedback session must be provided by the Clerkship Director (or their designate) at the approximate mid-point of the clerkship.
The Standard Departmental Examination format and cases (that are distributed at each faculty meeting) may be used for teaching as well as for formative and summative feedback, particularly in the assessment of clinical reasoning, problem solving and communications skills.
The patient encounter log should be reviewed at the time of the mid-core session. The mid-core feedback session must be a one-on-one session with each student with completion of the standard form, signed by both the Clerkship Director and the student. Summative evaluation of each student will include the administration of an end-of- core written examination in the form of the National Board of Medical Examiners Subject Examination in Surgery.
In addition to formative feedback given over the course of the 12-week rotation, a defined summative feedback session must be provided by the Clerkship Director (or their designate) at the conclusion of the clerkship.
CORE TOPIC GOALS and OBJECTIVES
In addition to general medical knowledge students will be required to demonstrate knowledge in all topics outlined in the AMBOSS study plan that will form the basis for learning within the clerkship. Please see the below topic learning objectives.
Module 1: Shock
- Define the types of shock: hypovolemic, septic, neurogenic, anaphylactic and cardiogenic.
- Describe the clinical signs of hypovolemic shock and relate them to the underlying pathophysiological process.
- Describe the critical objective measurements used to monitor the patient in shock.
- Describe the initial clinical management and resuscitation of the patient in shock.
Module 2: Trauma
- Explain the ATLS teaching of primary and secondary survey in the initial evaluation and treatment of acutely injured patients and define the classes of hemorrhage used in estimating loss of circulating blood volume.
- Describe the initial evaluation, stabilization, resuscitation and management of the patient with blunt and penetrating abdominal and thoracic trauma.
- Describe the initial evaluation, resuscitation and management of the patient with an isolated splenic injury.
Module 3: Head Injuries
- Explain the Glasgow coma score.
- Describe the principles of evaluation and treatment of head injuries including epidural and subdural hematoma.
Module 4: Burns
- Classify burns according to the depth of injury and etiology.
- Estimate the area of burn injury using the rule of nines.
- Describe the resuscitation of the burn patient using the Parkland Formula.
- Outline the basic principles of burn wound care.
Module 5: Acute Abdomen
- Outline the pathophysiology, clinical presentation and consequences of acute peritonitis, both localized and generalized.
- Describe the diagnosis and treatment of acute appendicitis, acute diverticulitis and acute perforated peptic ulcer.
- Develop a detailed understanding of the diagnosis and treatment of common biliary tract-associated causes of the acute abdomen including acute and chronic cholecystitis, cholangitis and acute pancreatitis.
- Describe the diagnosis and treatment of commonly occurring causes of the acute abdomen in infants and children including pyloric stenosis, intussusception and midgut volvulus.
Module 6: Intestinal Obstruction
- Differentiate large and small intestinal obstruction and list common causes of each condition.
- Differentiate intestinal obstruction from a dynamic (also referred to as paralytic) ileus.
- Explain the pathophysiology of fluid and electrolyte disturbances associated with small l intestinal obstruction.
- Describe the diagnosis, initial resuscitation and management options in the treatment of intestinal obstruction, including partial small intestinal obstruction, complete small intestinal obstruction, and colonic obstruction.
Module 7: Gastrointestinal Hemorrhage
- List the common etiologies of upper and lower gastrointestinal hemorrhage.
- Describe of the emergency diagnosis (including clinical examination, endoscopy and radiologic imaging), resuscitation and management of acute gastrointestinal hemorrhage.
- List the indications for surgical intervention in upper and lower gastrointestinal hemorrhage.
- Describe the pathophysiology of portal hypertension and the principles of management.
Module 8: Common Gastrointestinal and Cutaneous Malignancies
- Outline the steps involved in the clinical diagnosis and management of cutaneous malignancies.
- Outline the steps involved in the clinical diagnosis and management of gastrointestinal malignancies
- Demonstrate an understanding of the relevant anatomy that determines the strategy and extent of resection employed in the surgical management of gastrointestinal malignancies.
- Acquire an overview of the staging and prognosis of the common malignancies noted above.
Module 9: Hernias
- Define hernia and describe the different types of abdominal wall hernias.
- Demonstrate an understanding of the incidence, etiology, and complications, operative risks and rate of recurrence in the management of abdominal wall hernias.
- Outline the fundamental principles in the surgical management of inguinal, umbilical and abdominal incisional hernia.
- Define the terms related to abdominal wall hernias: reducible, irreducible, incarcerated, obstructed and strangulated.
Module 10. Surgery of the Breast
- Discuss the evaluation and management of common benign diseases of the breast.
- Describe the risk factor analysis, clinical examination, diagnosis and surgical management (both breast-conserving and breast-sacrificing) of in-situ and invasive malignancy of the breast.
- Describe the rationale for and technical approach to axillary lymph node management, including sentinel lymph node biopsy, in the surgical management of malignancy of the breast.
Module 11: Benign Colo-rectal Disorders
- Describe the diagnosis and treatment of common benign ano-rectal conditions including hemorrhoids, fissure-in-ano, fistula-in-ano, perianal abscess and peri-rectal abscess.
Module 12: Peripheral Arterial Disease
- Describe signs and symptoms of acute ruptured abdominal aortic aneurysm and describe the diagnosis, resuscitation and surgical management.
- Describe the pathophysiology and diagnosis, both non-invasive and invasive, and treatment of peripheral arterial occlusive disease.
- Describe the diagnosis and treatment of acute and chronic limb ischemia.
- Describe the signs and symptoms of cerebral transient ischemic attacks and outline the available diagnostic modalities, non-invasive and invasive, used in the evaluation of carotid artery disease.
- Describe the clinical course of mesenteric thromboembolic disease and discuss the approach to diagnosis and treatment.
Module 13: Venous Disease
- Review the venous system of the lower extremity and develop an understanding of the effect of tissue pressure, the significance of the muscle pump and the effect of valvular insufficiency.
- List the principles of management of varicose veins associated with venous insufficiency.
- Explain the pathophysiology of venous stasis ulcers of the extremities and the principles of their treatment.
- Describe the diagnosis and treatment of deep vein thrombosis (DVT), pulmonary embolism (PE) and the post-phlebitic syndrome.
Module 14: Thoracic Surgery
- Develop an understanding of the evaluation of a solitary lung nodule seen on chest imaging.
- List an overview of tumors commonly seen in the chest by location.
- Delineate the principles of surgical management of lung cancer.
- Develop an understanding of the commonly seen benign and malignant esophageal disorders including esophageal malignancy, achalasia and gastro-esophageal reflux disease (GERD).
Module 15: Transplant Surgery
- Develop an understanding of the status of transplant surgery in the USA and worldwide.
- Develop an understanding of the immunological aspects of transplant surgery including commonly used immunosuppressive medications and the side effects of immune-suppressive therapy.
- Define the terms, anatomic and biologic, used in the description of transplant donors and recipients.
Module 16: Laparoscopic Surgery
- Identify the comparative benefits and risks of laparoscopic surgery in comparison to open surgical procedures.
- Develop an understanding of advanced laparoscopic techniques and robotic surgery.
Module 17: Bariatric Surgery
- Define obesity and morbid obesity based on the body mass index (BMI).
- List the co-morbid conditions associated with morbid obesity.
Module 18: Endocrine Surgery
- Describe the symptoms, signs and management of hyperthyroidism.
- Discuss the evaluation of a thyroid nodule.
- Discuss the differential diagnosis and treatment of the patient with hypercalcemia.
- Discuss the pathophysiology of primary, secondary and tertiary hyperparathyroidism.
- Discuss the diagnosis and management of pheochromocytoma.
- Discuss the features of Multiple Endocrine Neoplasia (MEN) syndromes and their surgical treatment.
- Discuss the diagnosis and treatment of disorders of the pituitary adrenal axis.
Module 19: Ethical and Legal Issues in Surgery
a. Describe the principles of medical ethics applied to surgery including the concepts of patient advocacy, un-masking of economic influences and the duty to relieve suffering and ease pain with dignity.
b. Describe the fundamental elements of the patient-physician relationship.
c. Describe the responsibilities of the patient and the physician.
d. Discuss those aspects of medical ethics of particular concern to the surgeon:
1) “Futile” care
2) Organ procurement
3) Transplantation guidelines
4) Withholding or withdrawing care
5) HIV testing
6) Referral of patients
7) Confidentiality
8) Fee splitting
9) Informed consent
10) Substitution of surgeon
11) Disputes between medical supervisors and trainees
12) New medical and surgical procedures
Module 20: Surgery in the Elderly
Describe and explain the effect of the following factors on wound healing and recovery from illness, injury and operative treatment in elderly patients:
- Nutrition
- Metabolic state (including diabetes mellitus)
- Collagen synthesis and deposition
- Pharmacologic manipulation
- Physical activity/mobility
- Physiologic reserve and frailty
- Immune competence
Develop an understanding of the unique physiology and risk factors seen in the elderly in relation to the management of shock, trauma, head injuries, burns, the acute abdomen intestinal obstruction, common GI malignancies, hernias, surgery of the breast, venous disease, thoracic surgery, transplant surgery, laparoscopic and robotic surgery, bariatric surgery and endocrine surgery.
Module 21: Communication Skills in Surgery
Communication skills are critical to surgery in that surgical therapy is offered as an alternative to patients with whom a long-term professional relationship has not been previously developed. Students will:
- Learn to communicate effectively with patients, families, and the public, as appropriate, across a broad range of socioeconomic and cultural backgrounds particularly in regard to the concept of informed consent for surgical procedures.
- Describe the use of certified interpreters and language interpretation services in the process of informed consent for surgical procedures.
- Describe the unique aspects of effective communication with physicians, other health professionals, and health related agencies in association with surgical treatment and follow-up surgical care.
- Learn to work effectively as a member or leader of a health care team in surgery.
- Describe the consultative role of the surgeon to other physicians and health professionals.
- Learn to maintain comprehensive, timely, and legible medical records associated with surgical care.
SURGICAL SUBSPECIALTIES
ANESTHESIOLOGY:
- Discuss the pre-operative evaluation of the surgical patient in association with commonly occurring comorbid conditions.
- Discuss the intra-operative factors associated with anesthetic management, including intubation and airway management.
- Care and monitoring of the unconscious patient.
- Blood and fluid management.
- Local, regional and general anesthesia.
- Discuss the postoperative care of the surgical patient including:
- Monitoring in the post-anesthesia care unit (PACU)
- Pain management
- Early and late complications
- Discuss the toxicity of local anesthetics agents.
ORTHOPEDICS:
- Discuss the process of fracture healing.
- List common seen fractures of the long bones and pelvis.
- Outline the principles of immobilization of bones and joints in trauma.
- Delineate the diagnosis and treatment of low back pain and sciatica.
UROLOGY:
- List the common symptoms in the presentation of urinary problems.
- List the common urological problem encountered in clinical practice.
- Identify the methods used to treat ureteric and renal stones.
- Outline the diagnosis and management of benign and malignant prostate disease.
OPHTHALMOLOGY:
- Describe a normal fundoscopic examination and list the fundoscopic changes associated with common clinical conditions such as hypertension, diabetes and glaucoma.
- Describe the anatomy and pathophysiology of pupillary size and reactions in the diagnosis of neurologic abnormalities and head injury.
- Describe the symptoms and signs of glaucoma.
- Describe the management of minor eye trauma including subconjunctival hemorrhage and corneal abrasion.
OTORHINOLARYNGOLOGY:
Review the relevant clinical anatomy of ear/nose/throat.
Outline the diagnosis and management of common conditions of the ear including cerumen impaction, foreign body removal, and perforation of the tympanic membrane, Otitis external and Otitis media.
Develop an understanding of the common conditions of nose and sinuses including deviated septum, hyper-trophic turbinates, acute sinusitis and chronic sinusitis.
Develop an understanding of common surgically treated conditions of the throat including tonsillitis (and the indications for tonsillectomy) and obstructive sleep apnea (OSA).
WEB-BASED EDUCATIONAL ASSIGNMENTS FOR INDEPENDENT LEARNING
The school requires the successful completion of web-based assignments in order to receive credit for this clerkship. Students should log into Sakai and complete the following:
- SGUSOM's curriculum on AMBOSS
- UWorld
- Communication Modules
- Ethics Modules
- Geriatrics
The Office of the Dean monitors student performance on these assignments. The completion of these assignments will be sent to the Clerkship Directors for incorporation into the final clerkship grade. The clinical faculty feels these assignments are excellent preparation for the NBME clinical subject exams as well as Step 2. In addition, a student’s diligence in completing these assignments reflects a commitment to excellence, a component of professional behavior grade.
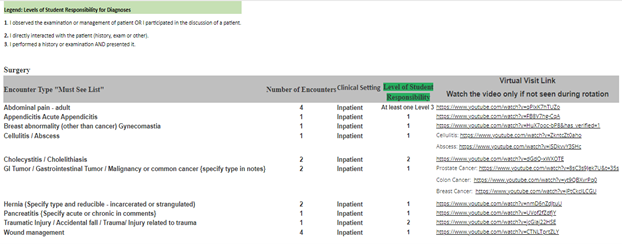
Required Clinical Encounters and the Patient Encounter Log
The below list of complaints and diagnoses must be entered into your Patient Encounter Log (PEL) Program during each Core and Family Medicine Clerkship.
Link: PEL https://myapps.sgu.edu/PEL/Admin/Account/Login?ReturnUrl=%2fPEL
The faculty in each specialty have identified specific clinical experiences that are a requirement for the clerkship. The PEL program is designed to track each student’s patient encounters, clinical setting in which the encounter occurs, and level of responsibility. This program allows the school to standardize the curriculum. All patient’s complaints and/or diagnosis encountered during clinical rotations must be entered into the PEL program. Entering the required clinical encounters “Must See List” is required during clinical rotations and will be displayed to the clerkship director for review on the final clerkship evaluation. Whenever possible incorporate the Communication Skill course topic for each required encounter. Never place patients’ names or any patient identifying information in this program, this would be a HIPPA violation.
If students are unable to see a required clinical encounter, they must view the virtual visit link and watch the video. Once the encounter video is viewed, add the virtual encounter in the PEL as a Virtual visit.
SURGERY READING LIST
REQUIRED
Print:
- Essentials of General Surgery and Essentials of Surgical Specialties
- Lawrence, Williams and Wilkins
RECOMMENDED
Books:
- Code of Medical Ethics Current Opinions with Annotations, AMA press.
- Early Diagnosis of the Acute Abdomen
Cope, Oxford University Press
- Essentials of Diagnosis and Treatment in Surgery
(Lange Current Essentials Series)
- The Ethics of Surgical Practice Cases, Dilemmas and Resolutions, Jones JW, McCullough LB and Richman BW, Oxford University Press.
- Lecture Notes: General Surgery
Ellis and Calne, Blackwell
- Principles of Surgery
Schwartz, McGraw Hill
- The ICU Book
Marino, Williams and Wilkins
Journals:
- Journal of the American College of Surgeons
Elsevier
- British Journal of Surgery
Wiley-Blackwell
Surgical Organizations:
Student membership in The American College of Surgeons is available through FACS.org, with the support of the Chair of Surgery, and is a well-developed source of educational material for the study of surgery.
WEB-BASED EDUCATIONAL ASSIGNMENTS FOR INDEPENDENT LEARNING
The school requires the successful completion of web-based assignments in order to receive credit for this clerkship. Students should log into Sakai to see these assignments. The Office of the Dean monitors student performance on these assignments. The completion of these assignments will be sent to the Clerkship Directors for incorporation into the final clerkship grade. The clinical faculty feels these assignments are excellent preparation for the NBME clinical subject exams as well as Step 2. In addition, a student’s diligence in completing these assignments reflects a commitment to excellence, a component of professional behavior grade.
