Mission and Goals
Mission: Our mission is to provide students a clinical experience that will prepare them to understand, evaluate and treat mental disorders in a context defined by knowledge, empathy and professionalism. The clerkship builds on a foundation of medical knowledge, adding clinical and communication skills to enable the student to understand behavioral problems using a biopsychosocial–cultural model, to formulate a well-supported differential diagnosis and to construct an effective treatment plan.
Goals: After completion of the six-week clerkship, students will:
- Demonstrate sufficient medical knowledge, clinical skill, clinical reasoning, communication skill and professional behavior required to participate in providing care for people with mental disorders in a multidisciplinary and diverse setting.
- Appreciate the multi-factorial aspects of health and illness in general, and the relationship between biological/medical, psychological, social and cultural aspects of health and illness that will enhance proficiency in clinical situations with all patients.
- Have the opportunity to decide if a career in psychiatry is right for them and receive guidance on succeeding in residency training and in professional development.
Educational Objectives: By the end of the clerkship, students will:
- Demonstrate knowledge of the epidemiology, pathophysiology, clinical findings, diagnostic criteria, diagnosis, differential diagnosis, and treatment of common mental disorders.
- Summarize the indications, mechanisms of action, typical side effects, drug interactions, and toxicities of psychotropic medications; most common drugs of abuse and their presentation; typical signs and symptoms of common psychopharmacologic emergencies and treatment strategies; indications and contraindications for ECT, as well as the clinical situations in which it may be a treatment of choice.
- Describe wellness and prevention strategies, principles, and common indications of the primary forms of psychotherapy.
- Discuss gender, race, immigration, socioeconomic status, and their effect on diagnosis, access to care, and healthcare disparities.
- Appraise levels of care, delivery methods (including telehealth), patient safety and quality improvement.
- Demonstrate respect for patient autonomy, privacy, and confidentiality, maintenance of professional boundaries, assessment of decisional capacity, and ability to obtain informed consent.
- Conduct a psychiatric interview.
- Perform a comprehensive or focused psychiatry history.
- Establish a therapeutic alliance with patients.
- Perform a mental status examination and, if needed, physical examination (including neurologic examination).
- Perform a cognitive evaluation using a structured evaluation tool (like the Mini-Mental Status Examination or the Montreal Cognitive Assessment).
- Conduct a suicide risk assessment and participate in a violence risk assessment.
- Prioritize a differential of DSM diagnoses based on history and examination.
- Discuss pertinent biopsychosocial factors in the patient's presentation.
- Describe appropriate diagnostic and management/treatment plans.
- Demonstrate evidence-based data and scientific literature search to answer pertinent clinical questions.
- Complete comprehensive and focused (or SOAP note) case write-ups documenting the history, examination, diagnosis, differential diagnosis, diagnostic, and treatment plan.
- Orally present comprehensive or concise cases.
- Demonstrate counselling and education to a patient or patient's family about participation in treatment, shared decision making, monitoring of clinical progress, diagnosis, and treatment.
- Demonstrate punctuality, reliability and responsibility, by attending and being prepared for all mandatory activities in a timely manner.
- Perform duties and assignments promptly and conscientiously as either a team member or a leader, playing an active role in patient care and academic activities.
- Demonstrate respect in interactions with staff, patients, families, and peers, using polite language and attitude, including in electronic communication.
- Demonstrate equity and sensitivity for patients of diverse backgrounds by treating patients of any age, race, sexual orientation, gender, disability, culture, and religion with compassion, empathy, humility, sensitivity, and tolerance and respecting others' time, rights, values, religious, ethnic, and socioeconomic backgrounds, lifestyles, opinions, and choices
- Display ethical behavior through adherence to school and institutional policies, adherence to professional boundaries, and upholding patient privacy and confidentiality.
- Demonstrate professionalism when handling complex situations such as conflicts, non-adherence, and other ethical dilemmas calmly, compassionately, and based on objective evidence, truthfulness, and justice.
- Demonstrate professional appearance and attire as defined by the school and institutional policies and appropriate demeaner by avoiding using electronic devices during patient care, lectures, and discussions.
- Demonstrate appropriate prudence by abstaining from using substances that compromise judgement and the ability to provide safe and effective care.
- Exhibit self-awareness and continuous growth by identifying personal strengths and weaknesses, acknowledging mistakes, and actively engaging in corrective actions using available academic and wellness resources.
- Seek and accept feedback to continually grow in knowledge, skills, and professionalism, acknowledging that a medical career requires life-long learning to maintain professional competence.
- Provide a genuine evaluation of educational activities, courses, and clinical rotations to improve the medical education curriculum.
The above objectives are met by engaging in a combination of didactic study and supervised clinical experience.
Didactic study:
- Classroom activities such as lectures, seminars, and student presentations.
- Self-directed learning activities such as Drexel Communication Skills Curriculum (doc.com), AMBOSS and UWorld.
Clinical experience:
- Assignment to one or more interdisciplinary clinical teams in a variety of clinical settings.
- Performing psychiatric evaluations and follow-up, including conducting a psychiatric interview and mental status examination, constructing a differential diagnosis according to the current diagnostic system, and formulating an effective treatment plan by participating in clinical activities with members of the team under the direction of preceptors.
Requirements: Students are expected to:
- Attend all assigned clinical and educational activities in their clinical area and in the department and observe work hours (Note: absences and leaving early can decrease professionalism grade).
- Be on call as assigned.
- Complete at least one comprehensive case write-up and two focused write-ups (SOAP Note) and submit them in a timely manner
- Complete assigned activities from the department’s web-based curriculum (AMBOSS, UWorld)
- Complete other assignments given by the preceptor, e.g. class presentations, making-up for absences or deficiencies.
- Complete modules 13 (managing strong emotions) and 15 (culture in the clinical interview) from the Drexel Communication Skills Curriculum (doc.com).
- Keep the patient electronic log current and bring a copy to the mid-core evaluation and submit a copy for the final evaluation.
- Do well on the final written exam (NBME subject exam).
Recommended Textbooks:
- Introductory Textbook of Psychiatry, Black and Andreasen, APP (currently in 6th edition)
- Study Guide to Introductory Psychiatry, Black & Cates, APP
- Synopsis of Psychiatry, Kaplan & Sadock, Wolters Kluwer (currently in 11th edition)
- Shorter Oxford Textbook of Psychiatry, Harrison & Cowen, Oxford University Press (currently in 7th edition)
- New Oxford Textbook of Psychiatry, Gelder, et al, Oxford University Press (currently in second edition)
- Psychiatry, Cutler & Marcus, Oxford University Press (currently in second edition)
Students are also encouraged to seek additional case-based reading, including journals such as the American Journal of Psychiatry, the British Journal of Psychiatry, as well as web-based resources and recommendations from preceptors (Up-to-Date, Medscape, etc.).
Study Guide: Please follow the AMBOSS study plan as a guide for the student in addition to other web-based curriculum.
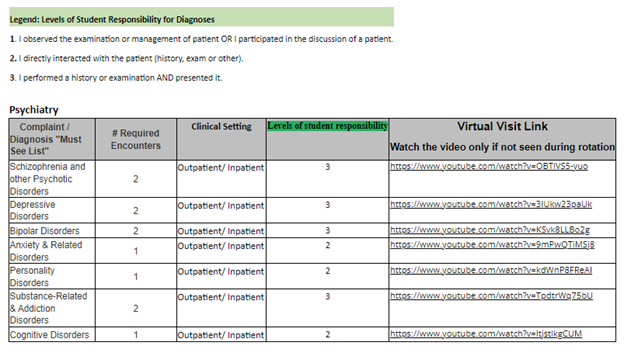
Required Clinical Encounters and the Patient Encounter Log
The below list of complaints and diagnoses must be entered into your Patient Encounter Log (PEL) Program during each Core and Family Medicine Clerkship.
Link: PEL https://myapps.sgu.edu/PEL/Admin/Account/Login?ReturnUrl=%2fPEL
The faculty in each specialty have identified specific clinical experiences that are a requirement for the clerkship. The PEL program is designed to track each student’s patient encounters, clinical setting in which the encounter occurs, and level of responsibility. This program allows the school to standardize the curriculum. All patient’s complaints and/or diagnosis encountered during clinical rotations must be entered into the PEL program. Entering the required clinical encounters “Must See List” is required during clinical rotations and will be displayed to the clerkship director for review on the final clerkship evaluation. Whenever possible incorporate the Communication Skill course topic for each required encounter. Never place patients’ names or any patient identifying information in this program, this would be a HIPPA violation.
If students are unable to see a required clinical encounter, they must view the virtual visit link and watch the video. Once the encounter video is viewed, add the virtual encounter in the PEL as a Virtual visit.
Student Midcore Evaluation Form Clerkship: PSYCHIATRY Rotation Start Date: Student: | St. George's University School of Medicine Hospital: Completion Date: Preceptor: |
THE FOLLOWING ITEMS WERE REVIEWED/DISCUSSED (check):
Log:________ “SOAP” note: ________ Doc.com _______ UWorld _______ AMBOSS________
One-Minute Preceptor Model (Modified) - A Guide for Providing Feedback
C- Commitment: How do you think you did?
P- Probe for supporting evidence: What went well and what are the areas to improve?
R- Reinforce the good (positive feedback); “I really like…”
G- Guidance on improving errors and omissions (correct mistakes): Here’s how you might try this in the future.
G- General rule: find a teaching point applicable to the situation
G- Goals for next time
SGUSOM Dept of Psychiatry "SOAP" Note Scoring Rubric (Use of Grading AND Feedback to Student)
