1. MISSION AND INTRODUCTION
Description of the Core Clerkship in Internal Medicine
The Medicine rotation teaches a logical and humanistic approach to patients and their problems. This process begins with a presenting complaint, through a comprehensive history and physical examination, to the formulation of a problem list, assessment of the problems including a differential diagnosis, a plan for definitive diagnosis and therapy, as well as an assessment of the patient’s educational needs.
While this sequence is applicable to all specialties in the clinical years, Medicine carries the major responsibility for teaching this clinical approach, thus forming the cornerstone of study in the clinical terms, regardless of a student’s future interests.
These twelve weeks expose the student to a wide range of medical problems. Skills in processing and presenting data to preceptors, peers and patients are assessed and refined. In addition, the clerkship introduces system-based practice, practice-based learning and improvement and cultural sensitivity and competency. The student learns the unique aspects of providing care for the elderly and those at the end of life. This includes the special needs of the elderly regarding multiple medication interactions, physical fragility and changes in cognition. The student learns interpersonal and communication skills and how to relate to patients, families and all members of the health care team in an ethical and professional manner.
Students accomplish the goals of the clerkship by extensive contact with many patients, conferences, lectures, bedside rounds and discussions with preceptors, residents and consultants, write-ups, case presentations, review of laboratory work, x-rays and imaging procedures, web-based educational programs as well as a prodigious amount of reading. The Department of Medicine places special emphasis on developing student skills not only in history taking, physical examination and written and oral case presentation, but also in understanding the pathophysiology of disease and in developing a problem list and a differential diagnosis. Humanism in Medicine is stressed throughout the clerkship as it will form an integral part of any physician’s life.
2. GUIDELINES
- Length: Twelve weeks.
- Site: In-hospital medical services and out-patient facilities. Students may also rotate through nursing homes, sub-acute nursing facilities or other similar places where healthcare is delivered.
- Orientation at the start of the clerkship: this should include an introduction to the key faculty and coordinators, a tour of the facilities, distribution of schedules, discussion of the expectations and responsibilities of the clerk, the general department and student schedule and the assignment to residency teams and preceptors. Students should be made aware of the contents of the CTM and the goals and expectations of the clerkship as a comprehensive learning experience. The SGU Clerkship Director in Medicine and preceptors are responsible to review and discuss the educational goals and objectives of the clerkship set forth in this manual before each rotation. In addition, there must be emphasis on developing communication skills, discussion of manual skills requirements and discussion of professional behavior.
- Schedule: All day Monday through Friday; night, weekend and holiday call with residency teams as assigned. Approximately 30% of the Clerkship should be allocated to protected academic time for teaching conferences and structured independent study.
- Attending rounds for house staff and students at least three times per week.
- A full schedule of teaching conferences including grand rounds, subspecialty conferences and didactic sessions pertinent to the needs of the students.
- Preceptor sessions at least four hours per week to include case presentation by students and beside rounds. These sessions should include a teaching physician and students only. At least one hour should be structured as a question-based session (MKSAP).
- Students are expected to complete 600 IM UWorld questions over the course of the 12-week rotation.
- A sufficient number of comprehensive write-ups are required over the course of the clerkship to ensure student competency in documentation of a comprehensive history and physical exam. These write-ups should include a comprehensive history, a physical exam, a review of relevant laboratory and imaging data, and a comprehensive problem list, with diagnostic, therapeutic and educational plans. This assessment should require considerable supplementary reading. The preceptor must read and critique these write-ups and return them to the student in a timely fashion. This timely interaction among faculty and student is an essential and core responsibility of the preceptor faculty. In addition, students must submit 2 “focused” write-ups – max 2 pages – based on clinical situations where a new problem arises in the course of hospitalization. These write-ups should include key historical features, relevant physical exam, pertinent laboratory data, and diagnostic assessment and plan for the patient. Students are required to present patient's pertinent history and physical findings orally during rounds and preceptor sessions to ensure student competency in oral presentation ability.
- A mid-term evaluation of each student’s performance is an important part of the rotation. This must include a review of the student’s patient log, a review of the student evaluations submitted by residents and attending who have had contact with the student, and a thorough discussion of the student’s strengths and weaknesses with advice as to how the student may improve. Students will also be expected to take a “practice” NBME shelf exam (self-evaluated) at the midpoint of the clerkship.
A final summative final assessment, conducted by the Clerkship director (or his/her designee), will be scheduled during the last week of the rotation. The final assessment will take in account the midcore, resident and preceptor feedback, review of PEL and required web-based courses.
3. EDUCATIONAL OBJECTIVES
The twelve-week core clerkship in internal medicine is based in acute care medical centers or appropriately designed and accredited ambulatory care facilities. The curriculum is designed to provide students with formal instruction and patient care experience so as to enable them to develop the knowledge, skills and behavior necessary to begin mastering the following clinical competencies essential to becoming a knowledgeable, complete and caring physician.
Students gain these and the additional skills outlined below by functioning as integral members of the patient care team, participating in resident work rounds and teaching attending bedside rounds every weekday and admitting patients when on-call and following them until discharge under the continuous supervision of the residents. Additional activities include meetings with their preceptors at least four hours per week (conferences for students only), attendance at daily didactic conferences and independent learning including completing web-based education assignments. An orientation at the start of the clerkship outlines the educational goals and objectives of the clerkship as well as the responsibilities of third year clerks, and assignments and schedules. Clerks are provided feedback regularly on their progress as well as during both midcourse and final summative reviews with their preceptor or clerkship director.
MEDICAL KNOWLEDGE
- Demonstrate knowledge of the principal syndromes and illnesses in Internal Medicine, their underlying causes both medically and socially and the various diagnostic and therapeutic options available to physicians in the care of their patients and in the care of populations.
- Develop an understanding of the cognitive processes inherent in clinical reasoning.
- Utilize the principles of diagnostic clinical reasoning, including translating patient information into medical terminology, becoming familiar with “illness scripts,” utilizing semantic qualifiers, and generating a prioritized differential diagnosis.
- Demonstrate knowledge of the indications for and the ability to interpret standard diagnostic tests, e.g.; CBC, chemistries, chest x-rays, urinalysis, EKGs, as well as other relevant specialized tests.
- Recognize unusual presentations of disease in elderly patients and demonstrate understanding of the complexity of providing care for the chronically ill with multiple medical problems. This should include an understanding of end-of-life issues, as well as bioethical, public health, epidemiologic, behavioral and economic considerations which arise in our health care system.
- Demonstrate knowledge of the indications for various levels of care post-discharge, e.g., short- and long-term rehabilitation, long-term skilled nursing facility care, hospice, home care, etc.
CLINICAL SKILLS
- Take a comprehensive history and perform a complete physical exam.
- Formulate a comprehensive problem list, differential diagnosis; and articulate a basic therapeutic plan, employing concern for risks, benefits, and costs.
- Analyze additional clinical information, lab tests and changes in patients’ clinical status; note changes in the differential diagnosis or in the diagnostic or therapeutic plans as circumstances and test results change.
- Begin to develop proficiency in basic procedures, such as venipuncture, arterial puncture, nasogastric tube insertion, insertion of intravenous lines, urinary bladder catheterization, etc.
COMMUNICATION SKILLS
Verbal:
- Basic competence in comprehensive case presentation
- Basic competence in focused case presentation
- Basic competence in explaining to a patient a simple diagnostic and therapeutic plan (e.g.; Community
- Acquired Pneumonia in a healthy 40 yr. old)
- Basic informed consent scenario for a procedure (e.g.; contrast enhanced CTS)
- Basic competence in safe transitions of care (i.e., sign outs, rounds and transfer of care)
Written:
- Competence in comprehensive case write-ups
- Competence in brief case write-ups (e.g. focused CS exercise)
- Communication (Drexel) Modules:
- Delivering Bad News
- Advance Care Planning
PROFESSIONAL BEHAVIOR
- Demonstrate a regimen of independent learning through the reading of suggested basic texts, research via the Internet and through other electronic resources, e.g., Up-To-Date, maintenance of the patient encounter log and completion of the web-based educational program requirements.
- Identify personal strengths and limitations.
- Demonstrate a commitment to quality, including awareness of errors, patient safety and self- directed improvement.
- Demonstrate competency and comfort in dealing with people of varying racial, cultural, and religious backgrounds
- Demonstrate a commitment to treating all patients, families and other caregivers with respect and advocate for their welfare.
- Participate fully with the patient care team and fulfill all responsibilities in a timely fashion.
- Maintain a professional appearance and demeanor.
- Demonstrate facility in working in concert with other caregivers including nutritionists, social workers and discharge planners to obtain optimal, seamless multidisciplinary care for patients, both during the hospitalization and after discharge.
4. CORE TOPICS & PATIENTS
Students should make every effort to see patients with conditions listed below. This list is based on “Training Problems “published by the Clerkship Directors of Internal Medicine.
- The healthy patient: health promotion and education, disease prevention and screening.
- Patients with a symptom, sign or abnormal laboratory value
- Abdominal pain
- Altered mental status
- Anemia
- Back pain
- Chest pain
- Cough
- Chronic pain
- Dyspepsia
- Dyspnea
- Dysuria
- Fever
- Fluid, electrolyte, and acid-base disorders
- GI bleeding
- Hemoptysis
- Irritable bowel
- Jaundice
- Knee pain
- Rash
- Upper respiratory complaints
- Weight loss
- Patients presenting with a known medical condition.
- Acute MI
- Acute renal failure and chronic kidney disease
- Asthma
- Common cancers
- COPD
- Diabetes mellitus
- Dyslipidemia
- CHF
- HIV
- Hypertension
- Inflammatory bowel disease
- Liver disease
- Nosocomial infection
- Obesity
- Peptic ulcer disease
- Pneumonia
- Skin and soft tissue infections
- Substance abuse
- Thyroid disease
- Venous thromboembolism
- Geriatric Issues
- Cognitive Impairment
- Osteoporosis
- Polypharmacy
- Incontinence
- Falls, gait and balance problems
- Failure to thrive
- Pressure ulcers
- Sensory impairments
- Sleep disorders
- Depression
- Pain
- Elder abuse and neglect
- End-of-life
5. READING
Reading should proceed on four levels, each with a different goal.
- Reading about your patient in order to “learn from your patients” and to develop a deeper understanding of the comprehensive issues affecting patient diagnosis and care.
- A systematic and thorough reading about the overall field of internal medicine in order to prepare for the end of clerkship shelf exam and the Step 2 CK. This cannot be over emphasized.
- Detailed in depth reading about specific topics of interest and for assignments.
- A review of basic science and relevant research in order to reinforce the fundamental principles of clinical medicine and understand advances in patient care.
- Students can choose from a large number of comprehensive texts book of medicine, medical sub-specialty texts, journal review articles and internet resources to read as outlined above.
6. WEB BASED EDUCATIONAL ASSIGNMENTS FOR INDEPENDENT LEARNING
The school requires the successful completion of web-based assignments:
- SGUSOM's curriculum on AMBOSS
- UWorld
- Communication modules
- Ethics Modules
- Geriatrics readings
Most web based assignments include Sakai quizzes that require a scores of 80% or greater in order to receive credit for this clerkship. Students are required to log into each clerkship’s Sakai site to see these assignments. The Office of the Dean monitors student performance on these assignments. The completion of these assignments will be sent to the Clerkship Directors for incorporation into the final clerkship grade. The clinical faculty feels these assignments are excellent preparation for the NBME clinical subject exams as well as Step 2. In addition, a student’s diligence in completing these assignments reflects a commitment to excellence, a component of professional behavior grade.
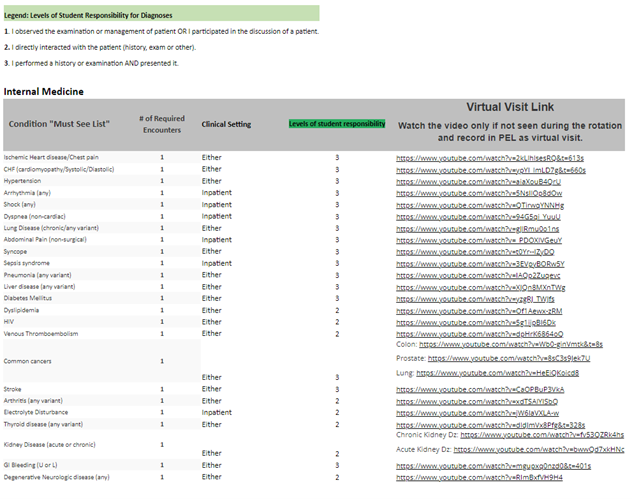
Required Clinical Encounters and the Patient Encounter Log
The below list of complaints and diagnoses must be entered into your Patient Encounter Log (PEL) Program during each Core and Family Medicine Clerkship
Link: PEL https://myapps.sgu.edu/PEL/Admin/Account/Login?ReturnUrl=%2fPEL
The faculty in each specialty have identified specific clinical experiences that are a requirement for the clerkship. The PEL program is designed to track each student’s patient encounters, clinical setting in which the encounter occurs, and level of responsibility. This program allows the school to standardize the curriculum. All patient’s complaints and/or diagnosis encountered during clinical rotations must be entered into the PEL program. Entering the required clinical encounters “Must See List” is required during clinical rotations and will be displayed to the clerkship director for review on the final clerkship evaluation. Whenever possible incorporate the Communication Skill course topic for each required encounter. Never place patients’ names or any patient identifying information in this program, this would be a HIPPA violation.
If students are unable to see a required clinical encounter, they must view the virtual visit link and watch the video. Once the encounter video is viewed, add the virtual encounter in the PEL as a Virtual visit.