CORE CLERKSHIP
MISSION AND INTRODUCTION
The clerkship in pediatrics provides a learning experience that fosters the highest standards of professional behavior based on principals of bioethics. It will provide students with a clinical experience that prepares them to communicate effectively with patients and families and learn to evaluate and manage children from newborn through adolescence.
The clerkship integrates a foundation of medical knowledge with clinical and communication skills to enable the student to identify and provide quality pediatric care.
After completion of a six week core rotation during the third year, students will demonstrate a firm understanding of the competencies required to evaluate and provide care for children who are sick and well.
The six-week core clerkship allows students to gain clinical experience in evaluating newborns, infants, children and adolescents, both sick and well, through clinical history taking, physical examination and the evaluation of laboratory data. Special emphasis is placed on: growth and development, nutrition, disorders of fluid and electrolytes, common infections, social issues, and preventative care including: immunizations, screening procedures, anticipatory guidance. The student will develop the necessary communication skills to inform, guide and educate patients and families.
Pediatric ambulatory and in-patient services provide an opportunity to observe and enter into the care of pediatric medical and surgical disorders. The student will learn how to approach the patient and family and communicate effectively as they take admission histories and perform physical examinations. They will then provide the patient and parents with the necessary information and guidance to understand and support the child through the time of illness. The student will learn age specific skills regarding interviewing pediatric patients and relating to their parents, and will develop the skills necessary to examine children from newborn through adolescence utilizing age appropriate techniques. The adequacy and accuracy of the students’ knowledge, communication skills, manual skills and professional behavior will be measured and evaluated by their supervising physicians, residents and preceptors. There will be formative evaluations and discussion of the students’ progress throughout the rotation with emphasis on a formal mid-core and end-core assessment.
It is expected that there be full and active participation in the multiple learning opportunities: didactic learning, clinical seminars, self-directed learning modules, patient rounds, conferences. Preceptor sessions are mandatory and take precedence over all other clinical activities. Students should excuse themselves from their other assignments and attend their preceptor session, unless excused by their preceptor. All of these components are designed to expand the student’s concept of how to provide quality care for pediatric patients.
In the out-patient services, the student learns the milestones of growth and development, infant feeding, child nutrition, preventative care (including immunization, screening procedures, and anticipatory guidance), the common ailments of childhood and diagnosis of rare and unusual illnesses. In the pediatric sub-specialty clinics, the student will observe the progression and participate in the management of a wide variety of serious and chronic pediatric illnesses.
Emergency department and urgent care experiences permit the student to be the first to evaluate infants and children with acute illnesses. Emphasis is placed on the evaluation of febrile illnesses, and common emergencies of childhood (e.g. poisonings, injuries).
The initial management of the newborn is learned in the delivery room. Students then practice the examination of the newborn and learn about the initiation of feeding, neonatal physiological changes, and common newborn conditions. In the newborn intensive care unit, the student is an observer of the management of the premature and term infant with serious illness. Emphasis is placed on observing and understanding the role of the pediatrician in the multidisciplinary team approach to critical care.
These experiences are designed to provide maximum contact between students and patients and their families. The student should use every opportunity to practice communication skills, improve their ability to perform accurate and concise histories, perform physical examinations, expand their knowledge of pediatric diseases, and attain skills in utilizing laboratory and radiologic evaluations most effectively.
GUIDELINES
- Length: Six weeks.
- Sites: General pediatric unit, ambulatory care unit, pediatric emergency department, nursery, NICU, PICU, private office practice, additional sites, as available.
- At the start of the clerkship an orientation is given. The SGU clerkship director or designee discusses the program’s goals and objectives, the responsibilities of the clerk, the schedule and assignments to preceptors and residents. The student is introduced to the key preceptors and staff members in the department.
- The student must participate in the night, weekend, and holiday on-call schedules. The clerkship director will set the number and timing of calls.
- The student must attend scheduled clinical conferences, grand rounds, subspecialty conferences, and learning sessions. Approximately 30% of the clerkship should be allocated to protected academic time for teaching conferences and structured independent study.
- A preceptor meets with students at least twice a week for a minimum of three hours per week. The preceptor sessions will include clinical discussions that focus on problem solving, decision making and adherence to bioethical principals.
- The student is involved in all patient care activities in the out-patient facility and inpatient unit.
- The student will be observed, and given immediate feedback, as they take a history and perform a physical examination on a newborn and a child.
- As an absolute minimum, each student should examine five term newborns. This includes reviewing the maternal medical record, performing a physical examination on the infant, and talking with the parent about basic care of the newborn and anticipatory guidance.
- Pediatric students have required clinical experiences that must be entered into the Patient encounter log. There is an additional requirement that medical students learn how to identify and report child abuse/neglect. There should be involvement in a case where a child is suspected as being the victim of child abuse/neglect or where the differential diagnosis includes child abuse/neglect. If such a case does not present itself, a virtual case may be used. There should be a discussion of the recognition and reporting requirement and the child protection response and services.
- Involvement in these cases should include taking a history, performing a physical examination, discussing the differential diagnosis, formulating a plan for laboratory/radiologic studies and deciding on a treatment plan. These cases may be from the inpatient units, the nursery, the Emergency Room, or the out-patient setting.
- Depending on circumstances, participation may be limited to that as an observer, especially in cases of sexual abuse, or the use of a virtual case.
- As an absolute minimum, each student will participate in the care of two adolescents. This includes taking a history and performing a physical examination as well as reviewing the immunization record and assessing the adolescent’s health, behavior, educational and environmental issues. It is preferable that one of the two adolescents described will have a chronic illness.
- The student will give at a minimum, one major presentation during the rotation. The presentation will be evaluated by the preceptor.
- A minimum of four complete clinical write-ups is required per student. These write-ups will be critiqued by the preceptor and returned to the student in a timely manner. It is preferable that the patients selected for these write-ups be examples of the case mix listed in guideline#9 above. The write-ups will be handed in at intervals during the rotation and returned promptly so that the student can improve their written expression.
- The student will keep a Patient Encounter Log. The log will list all of the patients that the student has had direct contact with. The log should reflect a commitment to accurate record keeping and reflect knowledge of the case.
- Each student will have a formative mid-core evaluation with a review of their Patient Encounter Log, case write-ups and AMBOSS quizzes to the session. The Log will be reviewed for completeness, quality and mix of cases. The student’s professional behavior will be addressed, as well as progress in attaining the knowledge and skills required to evaluate a patient. There will be appropriate comments and suggestions given to the student to guide them toward improvement.
- The student will use the patient encounter log to record manual skills and procedures performed or witnessed.
- The following procedures are recommended to be performed or witnessed during the Pediatric rotation:
- vision and hearing screening
- otoscopy
- administration of inhalation therapy (Metered Dose Inhaler/MDI/Spacer/Nebulizer).
- throat culture
- immunizations: intramuscular injection, subcutaneous injection.
- nasopharyngeal swab
- peak flow measurement
- The following procedures are recommended to be performed or witnessed during the Pediatric rotation:
- The students are responsible for completing the introductory modules of the Communication
- Skills course prior to the start of the 3rd year core rotations. In addition, the modules required for the pediatric rotation are:
- #21 Communication and Relationships with Children and Parents.
- #22 The Adolescent Interview.
- The student will complete the web-based assignments (see below) listed in Sakai.
- The final written examination will be the National Board of Medical Examiners (NBME) Clinical Subject Examination, given at designated sites.
- The Department of Pediatrics places special emphasis on professional behavior, as well as knowledge, interviewing skills, clinical problem solving and the ability to communicate information.
- The final grade is compiled from information gathered from preceptors, residents and staff Members who have evaluated the student’s professional behavior, knowledge, ability to communicate and clinical skills. The grade on the final written examination constitutes 30% of the final grade.
There are 5 components of the grade:
- Clinical Reasoning
- Clinical Skills
- Professional Behavior
- Communication Skills
- Written Examination – The student needs to score one standard deviation above the mean on the written examination to qualify for an A+ grade on the written examination.
When there is variation in the grades on the separate components, the final grade may be qualified with a + or a –.
An Honors grade (A+) will require an A in every component.
WEB BASED EDUCATIONAL ASSIGNMENTS FOR INDEPENDENT LEARNING
The school requires the successful completion of web-based assignments in order to receive credit for this clerkship. The following web-based courses are required:
- SGUSOM's curriculum on AMBOSS
- UWorld
- Communication Modules
- Ethics Modules
The Office of the Dean monitors student performance on these assignments. The completion of these assignments will be sent to the Clerkship Directors for incorporation into the final clerkship grade. The clinical faculty feels these assignments are excellent preparation for the NBME clinical subject exams as well as Step 2. In addition, a student’s diligence in completing these assignments reflects a commitment to excellence, a component of professional behavior grade.
- Apply knowledge of common acute and chronic pediatric conditions, congenital and genetic syndromes, including the importance of age on manifestations and treatment, in caring for patients, team discussions, and quantitative assessments.
- Describe major illnesses and conditions that affect newborns to their preceptors with epidemiology, signs and symptoms on presentation, treatment, and outcomes.
- Demonstrate knowledge of normal growth, development, and behavior.
- Discuss reporting norms and abnormalities in patient presentations (give examples of possible abnormalities in infancy through adolescence establishing the importance of these metrics).
- Demonstrate knowledge of health maintenance and preventative care for children including age related issues in nutrition, safety, immunizations and risk factor identification/modification, in various clinical settings.
- Demonstrate knowledge of nutritional requirements and feeding practices, noting the differences of each age and stage of childhood and proper documentation.
- Describe factors used in identifying child abuse and neglect.
- Discuss reporting requirements and available child protection response and services.
- Explain fluid and electrolyte requirements for patients, and the differences for patients of varying sizes and ages.
Clinical Skills
- Demonstrate empathy in age-appropriate communication with children and parents to form positive and informative relationships (Applying the Drexel University College of Medicine communications skills course).
- Demonstrate effective communication with a parent about basic care of the newborn with anticipatory guidance.
- Demonstrate a review of the records identifying and reporting pertinent information.
- Demonstrate skill in history gathering and interpreting relevant information in both acute and chronically ill patients in various clinical settings.
- Discuss laboratory data with age-appropriate norms in a healthcare team.
- Develop a problem list and formulate appropriate differential diagnoses.
- Develop treatment plans that consider the patient's identity, culture and ability to adhere to the recommendations.
- Demonstrate education on prevention and treatment of a disease.
- Present an accurate and organized diagnostic interview and physical exam and interpretation of tests.
- Create a summative assessment with documentation of reasoning and problem-based plans based on a patient interview.
- Develop a case presentation to accurately reflect the diagnosis(es), reason for the evaluation, the chronology of the history, the details of physical findings, the differential diagnosis and the development of an initial evaluation and plan.
- Perform a newborn exam.
- Describe the indications, consent (if warranted) and techniques of pediatric procedures.
- Discuss all required elements for safe transitions of care, discharge and follow-up plans.
- Discuss high risk births and perinatal treatments.
- Demonstrate information seeking skills by: Formulating a clinical question, utilizing the primary or secondary literature and assessing the credibility of information sources to answer the question, then sharing the information with the clinical team.
- Discuss the indications of utilizing pediatric healthcare system resources in providing patient centered care.
Professional Behavior
- Establish rapport with patients and families that demonstrates respect and compassion.
- Demonstrate honesty, integrity and respect in dealing with patients, families and colleagues.
- Adhere to the principles of confidentiality, privacy and informed consent.
- Demonstrate that you are a responsible team member and carry out all of your assigned duties in a timely manner.
- Demonstrate the ability to work effectively as a member of a health care team contributing to improved care.
- Demonstrate sensitivity to issues related to culture, race, age, gender, religion, sexual orientation and disabilities.
- Demonstrate the application of bioethical principles to respond appropriately to ethical dilemmas and conflicts, and uphold professionalism in all aspects of medical practice.
- Demonstrate responsibility in completing assignments.
- Recognize your personal biases and how they lead to diagnostic error.
- Demonstrate the indications for consultation.
- Demonstrate commitment to life-long learning.
- Develop a plan to strengthen deficiencies relevant to learning gaps identified through self-assessment of your own unique learning need.
CORE TOPICS
General
- Pediatric history
- Pediatric physical exam
- Patient write-up (problem oriented approach)
- Begin to formulate a differential diagnosis that relates to the presenting complaint, symptoms and findings on history and physical examination.
- Formulate a plan for further evaluation (i.e., laboratory, radiology), treatment and management.
Well Child Care
- Immunizations
- Routine screening tests
- Anticipatory guidance
- Nutrition
Growth and Development
- Developmental milestones (when and how to evaluate)
- Failure to thrive
- Short stature
- Obesity
Neonatology
- The normal newborn
- Neonatal problems (jaundice, respiratory distress, sepsis, feeding issues)
- Newborn screening
- APGAR scoring/Ballard scoring.
- Fetal Alcohol Syndrome
- Sudden Infant Death Syndrome
Common Childhood Illnesses and Their Treatments
1. Ear Nose and Throat (ENT) and pulmonary disorders
- Upper Respiratory Infection (URI)
- Asthma
- Pharyngitis
- Foreign body
- Otitis media
- Pneumonia
- Sinusitis
- Cystic fibrosis
- Cervical adenitis
- Tuberculosis
- Croup/epiglottitis
- Fever without focus
- Bronchiolitis
2. Eyes
- Conjunctivitis
- Ocular trauma
- Amblyopia
- Strabismus
3. Cardiac
- Fetal circulation
- Congenital anomalies: Ventricular Septal Defect (VSD), Atrial Septal Defect (ASD), Tetralogy of Fallot, transposition of the great vessels, coarctation of the aorta, patent ductus arteriosus (PDA), Pulmonic stenosis (PS). The significance of these defects as isolated findings and as they relate to genetic syndromes.
- Acquired heart disease: Rheumatic Fever (RF), myocarditis
- Hypertension
4. Gastrointestinal Disorders (G.I.)
- Gastroenteritis
- Constipation/Hirschsprung’s disease
- Acute abdomen (appendicitis, intussusception, volvulus)
- Inflammatory bowel disease
- Gastroesophageal reflux disease (GERD)
5. Endocrine
- Diabetes, Diabetic Ketoacidosis (DKA)
- Thyroid disease
- Adrenal disease
- Congenital Adrenal Hyperplasia (CAH)
- Failure to Thrive
- Obesity
- Metabolic Syndrome
6. Neurology
- Seizures
- Meningitis
- Head trauma
- Cerebral palsy
- Tumors
7. Hematology/Oncology
- Anemias/hemoglobinopathies
- Pediatric malignancies (Acute Lymphatic Leukemia, lymphomas, neuroblastoma, Wilm’s tumor)
- Immune thrombocytopenic purpura (ITP)
8. Renal and Genitourinary (G.U.)
- Urinary tract infections (UTIs)
- Nephritis/nephrosis
- Fluid and electrolyte balance
- Congenital anomalies
9. Dermatology
- Seborrheic dermatitis
- Atopic dermatitis
- Impetigo
- Fungal Infections
- Exanthems
- Neurocutaneous stigmata (neurofibromatosis, etc.)
10. Ingestions and Toxidromes
- Lead poisoning
- Salicylate, acetaminophen
- Iron
11. Common Pediatric Orthopedic Problems
- Developmental dysplasia of the hip
- Osgood Schlatter
- Slipped Capital Femoral Epiphysis
- Torsions
- Legg-Calve-Perthes disease
- Dislocated radial head (Nursemaid’s elbow)
- Fractures
12. Musculoskeletal System
- Osteomyelitis/septic arthritis
- Muscular dystrophies
13. Adolescence
- Tanner staging
- Precocious/delayed puberty
- Stages of adolescent development
- Sexually transmitted infections
- Pregnancy/menstrual irregularities
- Vaginal discharge
14. Child Maltreatment Syndrome
- Physical abuse
- Sexual abuse
- Emotional abuse
- Neglect
15. Genetics
- Down Syndrome, #21 trisomy
- #13 trisomy
- #18 trisomy
- Turner Syndrome
- Klinefelter Syndrome
16. Collagen Vascular
- Juvenile Rheumatoid Arthritis
- Systemic Lupus Erythematosus
- Henoch Schonlein purpura
- Kawasaki disease
- Hemolytic Uremic Syndrome
17. Behavioral Issues
- Temper tantrums
- Discipline issues
- Sleep disorders
- Attention Deficit Disorders
- Hyperactivity issues
- Learning disabilities
- Oppositional defiant disorders
18. Immunology
- Human Immunodeficiency Virus infection (HIV)
- Congenital Immunodeficiency Syndromes
19. Ethical Principals
- Respect for persons (privacy, confidentiality, informed consent, inclusion of patient/parent
- In decision making, provision for identity and culture, disclosure)
- Medical beneficence (concern for the patient’s best interest)
- Non-maleficence (not harming)
- Utility (balancing potential benefit to potential harm)
- Justice (being fair)
READING
Suggested Approach to Reading for Medical Student Pediatric Rotations
“Reading” is an essential part of medical education. How to best benefit from the time spent reading for Pediatrics may vary among individuals. More important, than the reading per se is the retention of what you have read and the ability to recall and return to the source of the material – to create a “library” of important material in your notes in your files, and in your memory.
The following suggested reading materials (comprehensive textbooks, condensed textbook, specialized topical books, reference books, synopses, journals, internet sites) may be available at your Pediatric site and should constitute sufficient resources for your basic and applied Pediatric reading.
As you start your rotations, important preliminary reading should be done in the earlier chapters devoted to Growth and Development in one of the comprehensive textbooks. One must formulate a sense of the normal parameters of each stage of development so as to appreciate how illness affects children differently during different stages of the pediatric years.
These textbooks, journals, as well as internet sites, provide in-depth descriptions of all new aspects of pediatric care.
Students should use the most recent edition of the following:
Required
- Pediatrics for Medical Students – Most recent edition, edited by Daniel Bernstein and Steven P. Shelov, Lippincott Williams and Wilkins
Comprehensive Textbooks
- Nelson’s Textbook of Pediatrics, Latest Edition, Saunders publisher, edited by Behrman, Kliegman, Jenson
- Rudolph’s Textbook of Pediatrics, Latest Edition, McGraw-Hill publisher, edited by Rudolph, Rudolph, Hostetter, Lister, Siegel
- Illustrated Textbook of Pediatrics by Tom Lissauer and Graham Clayden
- Pediatrics and Child Health by Rudolf and Levene published by Blackwell
Condensed Textbooks
- Pediatrics: A Primary Care Approach, 1st Edition, Saunders publisher, Editor C. Berkowitz
- Manual of Pediatric Practice, Saunders publisher, Editor L. Finberg
- Growth and Development, Watson and Lowrey
- Essential Pediatrics, Hull and Johnstone
Useful Subspecialty Books
- Textbook of Pediatric Emergency Medicine, Lippincott, WW publisher, edited by Fleisher, Ludwig, Henretig, Ruddy, Silverman
- Clinical Pediatric Dermatology, Elsevier publisher, edited by Paller & Mancini
- Atlas of Pediatric Physical Diagnosis, Mosby publisher, edited by Zitelli and Davis
- The Requisites in Pediatrics, Mosby publisher, series of small topical subspecialty volumes edited by L Bell, including Nephrology, Urology, Pulmonary, Endocrinology, and Cardiology
- Red Book, (Infectious Diseases) American Academy of Pediatrics, Edited by Pickering et al
Abbreviated Reference Books
- Harriet Lane Handbook, Mosby publisher, edited by senior pediatric residents at The Johns Hopkins Hospital
- Pediatric Secrets, Hanley & Bellis publisher, edited by Polin and Ditmar
- The 5-Minute Pediatric Consult Series, CHOP, edited by M. William Schwartz
Resource Materials pertaining to Cultural Competency
- Bigby J. Cross Cultural Medicine. New York: American College of Physicians, 2003 p. 1-28
- Miller S.Z. Humanism and Medicine Acad Med Vol 74, N07/July 1999 p. 800-803
- Coulehan JL. Block MR. The Medical Interview; Mastering Skills for Clinical Practice. 4th edition
- Philadelphia, Davis, 2001. Chapter 12 Cultural Competence in the Interview p. 228-245
- The Spirit Catches you and You Fall Down; A Hmong Child, Her American Doctors, and the Collision of Two Cultures. By Anne Fadiman. Farrar, Straus
Journals
- Pediatrics
- Journal of Pediatrics
- Academic Pediatrics
- Pediatrics in Review
- Pediatric Clinics
- Journal of Pediatric Infectious Disease
Internet Sites
- www.comsep.org - Provides curriculum and lists topics in pediatrics. This site is primarily for faculty members, but has relevant sections for students. Includes excellent video demonstrating how to perform a physical examination on a child.
- www.aap.org - Offers access to all American Academy of Pediatrics Policies and Guidelines
- https://www.aap.org/en/practice-management/bright-futures - Offers information about developmental milestones, anticipatory guidance, and mental health
- www.ncbi.nlm.nih.gov/books/NBK1116/ - Sponsors a database for genetic diseases and newborn screening methodologies
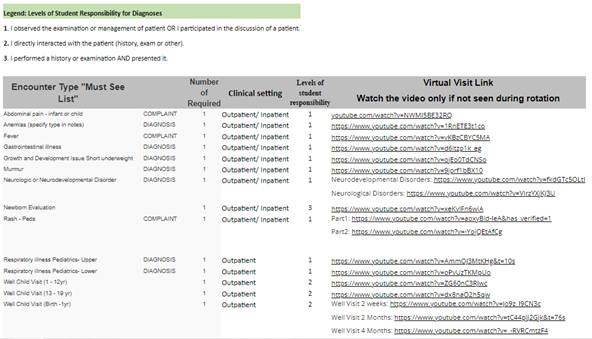
Required Clinical Encounters and the Patient Encounter Log
The below list of complaints and diagnoses must be entered into your Patient Encounter Log (PEL) Program during each Core and Family Medicine Clerkship.
Link: PEL https://myapps.sgu.edu/PEL/Admin/Account/Login?ReturnUrl=%2fPEL
The faculty in each specialty have identified specific clinical experiences that are a requirement for the clerkship. The PEL program is designed to track each student’s patient encounters, clinical setting in which the encounter occurs, and level of responsibility. This program allows the school to standardize the curriculum. All patient’s complaints and/or diagnosis encountered during clinical rotations must be entered into the PEL program. Entering the required clinical encounters “Must See List” is required during clinical rotations and will be displayed to the clerkship director for review on the final clerkship evaluation. Whenever possible incorporate the Communication Skill course topic for each required encounter. Never place patients’ names or any patient identifying information in this program, this would be a HIPPA violation.
If students are unable to see a required clinical encounter, they must view the virtual visit link and watch the video. Once the encounter video is viewed, add the virtual encounter in the PEL as a Virtual visit.